Common acne (aka "acne vulgaris") is a skin condition characterized by what are often called pimples or zits. It can occur anywhere on the body and at any age, though it typically affects teenagers on the face and back. You can take steps to avoid and prevent acne, as well as keeping yourself healthy and presentable, by doing the following.
- Remove dead skin cells regularly by exfoliating. Use an abrasive cloth or scrub, or use an over-the-counter chemical exfoliant like salicylic acid and glycolic acid. Remember that over-exfoliating can actually increase the likelihood of red, dry skin by irritating the skin.
- Remove bacteria from your pores. Your skin can become "allergic" to this bacteria. Use bactericidal products containing benzoyl peroxide by rubbing, twice daily, into the pores over the affected region or washing with a medicated soap bar/wash. Keep in mind that this may cause dryness, local irritation and redness.
- Avoid exposing your skin to other sources of oil and irritants.
- Break the habit of touching your face.
- Keep bangs off of your forehead--the oil and the hair products (if any) can clog pores.
- If you use a phone a lot, don't let it touch your face.
- Change your pillowcases and sheets once a week to prevent the build-up of oils and bacteria that can re-occupy your pores.
- Use non-comedogenic moisturizers and makeup. Choose cosmetics that are water-based and hypoallergenic. Avoid oil-free products, coal tar derivatives, and heavy creams. Make sure you wash your skin thoroughly every night to remove makeup residue.
- Review your diet and the research surrounding the links between diet and acne. The relationship between food and acne is a debatable topic. Your diet may or may not have an effect on acne.
- Studies have shown a correlation between milk and acne. Try substituting with soy milk and other calcium-rich foods.
- Excessive consumption of foods high in iodine (e.g. some seafood) may worsen acne but probably won't trigger it
- Research suggests--but does not prove--that a diet with a low glycemic index may reduce the likelihood of acne. High glycemic foods to replace with healthier alternatives include:
- soft drinks (drink water instead)
- sweets (substitute with fruit)
- white bread (replace with whole wheat bread)
- Remove other potential causes of acne. Some factors, such as being in puberty, can't be altered, but these can, with the approval of your doctor:
- Try asking a skin doctor also known as a dermatologist about your acne
- Minimize use of medication containing halogens (iodides, chlorides, bromides), lithium, barbiturates, or androgens
- Keep your bedsheets clean. Wash your pillow case on a regular schedule to reduce the transfer of natural body oils.
- Wash your face at least two times a day. Use face washes such as Neutrogena Oil Free Acne Wash or other face washes.
- There are no perfect creams or medicines that make your face smooth, soft and acne-free.
Tips
- Watch your diet and observe the effects it has on your skin. Whatever science has to say, every body is different and how yours responds to certain conditions can best be determined by you alone. As with any common condition, keeping your body hydrated is sound advice.
- Sometimes the best way of taking care of this condition is by doing it naturally, as in using natural products. Recommended are some such as : Witch Hazel, to be applied with a cotton swab after washing face. Dr. Bronner's Tea Tree Body Soap, which because of its Tea Tree elements, can reduce pimples on the face quite well if used at least twice a day.
- Neutrogena is a good product that can prevent or treat acne! it is sold at any drugstore.
- If you can afford it, I highly reccomend this place called Skinprint (I don't know where all of the branches are but there is one in Red Bank, New Jersey) They mix a face wash, moisterizer, and other products that are perfect for your skin, they test it in the beginning. The only problem is it's expensive, but it's worth it.
Warnings
- Do not make any drastic changes in your diet or skin routine without first consulting a medical professional.
- Anything beyond very gentle cleansing can actually worsen existing lesions and even encourage new ones by damaging or overdrying skin.
- You should only scrub your face if you have no existing pimples. Scrub lightly; avoid scrubbing too much or with too much pressure.
- Benzoyl peroxide can have a bleaching effect on clothes and hair. It may also increases sensitivity to the sun, so you might find that you burn faster!
Treating Pimples
How to remove pimples? These are a couple of things people actually do.
1. Use Acne Products
Here are a few basic tips on how to get rid of acne.
Don’t pick or press your pimples. If you do you will spread the bacteria under the skin which will promote swelling and increase your risk of scaring. Actually if you really can’t help it, there is a way to do this properly so as not to spread the bacteria but it is not advisable.
Wash once or twice a day. But go easy, washing with soap only removes the oil from surface and not the blocked pores. Use an oil free anti-bacterial face wash containing salicylic acid such as clearpores. Washing goes well with treating pimples as well as preventing pimples. Make this a daily habit.
It is advisable to avoid touching your face. Our hands are full of bacteric. Touching your face will simply help the bacteria spread on your face. This is something that is hard to avoid so be sure to always wash your hands.Use a water based product containing salicylic acid(2%) and SD alcohol 40 (1%). These medications are used as skin treatments to treat acne, remove warts and to treat psoriasis and other skin conditions. Dermatologists recommend 2% of salicylic acid as the perfect amount to treat acne.
Don’t wait if you have pimples. You have to treat acne as early as possible. In case you already have pimple scars, microdermabrasion or laser skin resurfacing can help.
Pimples
Acne is the term used for pimples and complexion problems wich can occur in young people and some adults. Pimples usually occur on the face, but may involve the neck,the arms, the chest or the neck. Acne is only a skin problem. It does not affect your general health.
Causes? At puberty, the oil glands of the skin start producing an oily material. It is called sebum. Sebum lubricates the skin. In some cases, the wall of the oil gland breaks and spills the sebum within the skin. That causes redness,swelling, and pus. In other words a pimple. Plugged oil glands may form whiteheads and blackheads. Blackheads are not caused by dirt. There is a bacteria that normally lives on the skin called Propionibacterium acnes. This bacteria lives on the sebum produced by the skin oil glands. Sometimes, this bacteria multiplies and causes inflammation and acne. Pimples are built into your genes it runs in families. In women, acne frequently worsens at the time of menstruation. Foods do not cause pimples! But there are cases when certain foods will make pimples worse. The most common ones are chocolate, milk, nuts or carbonated beverages. Acne may become worse under stress. Cosmetics make acne worse. Adult women often have trouble with acne through middle age. The reason is unknown.
The best way in treating pimples is to use benzoyl peroxide 5% gel (available at your local drug store) to the involved areas at night and NeoStrata alpha hydroxyacid in the morning (without using prescription medication). Some people are allergic to benzoyl peroxide. A product named Tend Skin is an effective acne treatment. Another advice is to wash your face twice a day with a mild non-soap cleanser. Do not pick or squeeze your pimples, as it can leave scars. Acne surgery can be done using sterile instruments to remove blackheads, whiteheads, and pimples.
There is no medical cure for acne. Acne can be controlled, but not cured. Many people do outgrow acne. Altough it is not recommended,sunlight may help some acne patients. Sunlight causes aging, wrinkling of the skin, and skin cancer. If cosmetics are used, they should be oil-free (the kind that separates into two layers). Cosmetics labeled water-based may still contain oil. If a moisturizer is used, it should be labeled non-comedogenic which means does not cause pimples.Your dermatologist may prescribe antibiotics to take by mouth,or to put on the skin.
Retin-A can also be used on the skin, even on body pimples. An effective acne regimen is two combine Retin-A with glycolic acid peels every few weeks. This involves coming to the office every two weeks to have a weak acid applied to the face. The acid removes the surface material from the skin that causes pimples to form. The face is left red and irritated for a few days. Once your acne is under control, the glycolic acid peels only need to be done every three months or so. When you come in for a light peel, the esthetician can also remove any blackheads or whiteheads that are found.
Beta hydroxyacid peels also are effective for treating acne.Accutane is a drug taken by mouth which is reserved for severe acne. Accutane has many side effects and if taken during pregnancy will cause birth defects. Patients taking Accutane must have periodic blood tests and checkups.
In conclusion,there are many different treatments for acne. Not all people respond to the same treatments. If the first medications do not work, chances are the second ones will.
About the Author
John Eminescu is a 29 years old writer. He work for a local newspaper and wrote 2 books about skin diseases.
Acne
This factsheet is for people who have acne.
Acne is a skin condition that causes spots. Most people affected by acne are aged between 12 and 25.1 However, men and women in their 30s and 40s can also suffer. There are many treatments available to help deal with the condition.
What is acne?
Acne is a skin condition that typically causes one or more of the following:
- blackheads (comedones) 2,3
- whiteheads2,3
- red or yellow spots2,3
- greasy skin2,3
- scars2,3
Acne typically affects the skin of the face, back, neck, chest and arms and the severity of the condition can vary.1,4
Acne affects people of all skin colours. The processes that cause acne are exactly the same in people with black or brown skin but the impact is altered by the skin pigmentation.
Acne is very common and affects about 80 in 100 people aged 11-30 at some time.4
The skin
The surface of the skin has lots of small sebaceous glands just below the surface. These glands make an oily substance called sebum that keeps the skin smooth and supple.
Tiny pores (holes in the skin) allow the sebum to come to the skin surface. Hairs also grow through these pores.

Illustration showing the structure of skin
What causes acne?
Acne is caused by the overactivity of the sebaceous glands that secrete oily substances onto the skin.
The sebaceous glands of people with acne are especially sensitive to normal blood levels of a hormone called testosterone, found naturally in both men and women.
Testosterone in people prone to acne triggers the sebaceous glands to produce an excess of sebum. At the same time, the dead skin cells lining the openings of the hair follicles (the tubes that hold the hair) are not shed properly and clog up the follicles.
These two effects combined cause a build-up of oil in the hair follicles. This causes blackheads and whiteheads to form.
For some people, their acne does not progress beyond this stage.
However in other people, the build-up of oil in the hair follicles creates an ideal environment for a bacterium called Propionibacterium acnes to grow.
These bacteria normally live harmlessly on your skin but when this ideal environment is created, they grow. They feed off the sebum and produce substances that cause a response from your body's immune system. This inflames the skin and creates the redness associated with spots.
In more severe 'inflammatory acne', cysts develop beneath the skin's surface. These acne cysts can rupture, spreading the infection into nearby skin tissue. This can result in scarring.
Acne myths
Contrary to popular belief acne is not caused by:
- eating fatty food or chocolate1
- dirt - blackheads get their dark colour through excess skin pigment - not dirt so washing more does not help, although if you do not wash your skin at all, bacteria will be able to multiply1,5
Acne is not contagious, so you cannot catch it.1
What makes acne worse?
There are a number of things that can make your acne worse. These include the following:
- picking and squeezing the spots may cause further inflammation and scarring1
- stress can make acne worse in some people, although it is not clear why1,5
- in women, outbreaks may be affected by the hormonal changes that occur during the menstrual cycle1,5
- excessive production of male hormones such as testosterone from conditions such as polycystic ovary syndrome may be another cause.5 For more information, please see the separate BUPA factsheet Polycystic ovary syndrome
- some contraceptive pills may make acne worse. This is due to the type of progestogen hormone in some pills whereas some other types of contraceptive pills can improve acne - see Treatments section below. Your GP will advise you which contraceptive pill to take1,5
- some medicines can make acne worse. For example, some medicines taken for epilepsy, and steroid creams and ointments that are used for eczema. Do not stop a prescribed medicine if you suspect it is making your acne worse, but tell your GP. An alternative may be an option1,5
- steroids can cause acne as a side-effect1,5
Diagnosing acne
Acne is easily recognised by the appearance of the spots, and by their distribution on the body.
There are several varieties of acne and your doctor will be able to tell you which type you have after examining your skin.
Treatment
Acne may cause you considerable emotional distress but there is a range of treatment options to help you tackle the problem. No treatment will completely 'cure' your acne. The aims of treatment are to prevent new spots forming, to improve those already present, and to prevent scarring.3
Home treatment
It is important to keep spot-prone areas clean, so wash the affected area twice a day with an unperfumed cleanser.1,6 The skin needs a certain amount of oil to maintain its natural condition, so avoid aggressive washing with strong soaps.
There are a number of over-the-counter remedies available from pharmacies to treat mild acne. These usually contain antibacterial agents such as benzoyl peroxide (eg Oxy and Clearasil Max).
As well as its antibacterial effects, benzoyl peroxide can dry out the skin and encourage it to shed the surface layer of dead skin. Together, these effects make it harder for pores to become blocked and for infection to develop.
Benzoyl peroxide can cause redness and peeling, especially to start with. This tends to settle down if you reduce the number of times you use it. You can then build up your use gradually.7
No home treatments for acne will work immediately. It can take weeks, if not months, for significant effects to be noticeable. If home treatments have not worked after two months, or you have severe acne, you should visit your GP.7
Prescription medicines
Your GP may start your treatment by prescribing a preparation containing benzoyl peroxide. If this does not work, or if you have more severe acne, there are a range of other treatment options that you can either rub onto your skin (topical) or take in tablet form (oral).
Topical treatments
There are several topical treatments you may be prescribed including those listed below:
- azelaic acid (Skinoren) is an alternative to benzoyl peroxide and may not make your skin as sore as benzoyl peroxide7
- topical retinoids (eg Adapalene) are medicines based on vitamin A, which are rubbed into the skin once or twice a day.7 They work by encouraging the outer layer of skin to flake off
- a topical antibiotic lotion applied to the skin can be used to control the P. acnes bacteria (eg Dalacin T). Treatment needs to continue for at least six months. Preparations that combine an antibiotic with other acne medication are available (eg Benzamycin which combines an antibiotic with benzoyl peroxide)7
Oral treatments
There are several oral treatments you may be prescribed including those listed below:
- oral antibiotics (tablets), such as tetracycline, can be prescribed for inflammatory acne. They should be taken daily for around three months, although it might take four to six months for the benefits to be seen.7 The success of this treatment can be limited because the strains of bacteria are often resistant to the common antibiotics. Antibiotics do not prevent pores from becoming blocked so treatment to prevent blackheads, such as benzoyl peroxide, is often also prescribed at the same time
- some types of oral contraceptive tablets help women who have acne. A combination of the usual pill hormone called ethinylestradiol with cyproterone acetate (eg Dianette) suppresses male hormone activity so is often used in women with acne4,7
- isotretinoin (eg Roaccutane) is a medicine known as an oral retinoid, which also exists in a topical form (see above). Isotretinoin works by drying up oily secretions. It tends to be prescribed to people with severe forms of acne that have proved resistant to other treatments. There a number of serious side-effects of this drug, such as liver disorders and depresssion.3,7 You should not take isotretinoin if you are pregnant, as it is very dangerous to an unborn baby.7 For safety reasons, isotretinoin is only prescribed under the supervision of dermatology specialists
Whitehead acne
Whiteheads are the direct result of skin pores becoming clogged with sebum (naturally occurring oil) and dead skin cells. Once this combination of dead skin cells and sebum combine with bacteria the result is an infection. The infection remains below the surface of the skin forming a whitehead. There are several treatments used to treat acne, including benzoyl peroxide, salicylic acid, and herbal treatments
Blackhead

A blackhead (medically known as an open comedo[1] , plural comedones [2]) is a yellowish or blackish bump or plug on the skin. A blackhead is a type of acne vulgaris. It is caused by excess oils that have accumulated in the sebaceous gland's duct. Blackheads are typically caused by excessive oil and makeup, which can facilitate the multiplication of the bacterium Propionibacterium acnes, the predominant anaerobe of the normal skin flora.[citation needed] The substance found in these bumps mostly consists of keratin and modified sebum (an oily secretion of the sebaceous gland), which darkens (resembling dirt) as it oxidizes. [3]
For information on the causes and treatment of blackheads, see the above linked acne vulgaris.
Acne vulgaris
Acne Vulgaris is an inflammatory disease of the skin, caused by changes in the pilosebaceous units (skin structures consisting of a hair follicle and its associated sebaceous gland). Acne lesions are commonly referred to as pimples, spots, or "zits".
Acne develops because of impairments of the functioning of skin glands (dermis and epidermis), notably blocked follicles.
 | |
|---|---|
| Acne of a 14 year old boy during puberty | |
| ICD-10 | L70.0 |
| ICD-9 | 706.1 |
| DiseasesDB | 10765 |
| MedlinePlus | 000873 |
| eMedicine | derm/2 |
Sufferers experience itching and discomfort due to swelling and bacterial overgrowth inside infected glands and adjacent cells, and try to relieve the swelling by squeezing acne with their fingers rather than clinically with a sharp sterilised needle. Damage to underlying layers of flesh destroys the integrity of the dermis and creates a weak zone to be attacked by bacteria, and an immune response resulting in more acne draining into the surrounding sebaceous glands. Bruising can also scar and deform the fine structures of the dermis so that its function is impaired and can create longer term havens for bacteria.
The fine structure of the dermis is very intricate, with dozens of specialized cells, sweat glands, oil glands, nerves and capillaries. it is subject to malformation, damage, and infection. Some sebaceous glands grow deformed without a drainage channel through the skin. Others swell by up to 20 times their original size. When these are drained, the walls of the enlarged gland are still intact under the skin and free to accumulate sebum and may or may not become infected. Sometimes a pustule forms around a hair strand that has not reached the surface and that has grown more than a centimetre curled inside the sebaceous gland.
Acne is a highly complicated and variable form of skin infection. It is most common during adolescence, affecting more than 85% of teenagers, but not infrequently also continues into adulthood.[1] For most people, acne diminishes over time and tends to disappear, or at least decrease, after one reaches his or her early twenties. There is, however, no way to predict how long it will take for it to disappear entirely, and some individuals will continue to suffer from acne decades later, into their thirties and forties and even beyond.

The term acne comes from a corruption of the Greek άκμή (acme in the sense of a skin eruption) in the writings of Aëtius Amidenus. The vernacular term bacne or backne is often used to indicate acne found specifically on one's back.
The most common form of acne is known as "acne vulgaris", meaning "common acne." Many teenagers get this type of acne. Excessive secretion of oils from the sebaceous glands accompanies the plugging of the pores with naturally occurring dead skin cells (corneocytes) blocking hair follicles. The accumulation of these corneocytes in the duct appears to be due to a failure of the normal keratinization process in the skin which usually leads to shedding of skin cells lining the pores. Oil secretions are said to build up beneath the blocked pore, providing a perfect environment for the skin bacteria Propionibacterium acnes and the lipophilic (oil/lipid-loving) yeast Malassezia[citation needed] to multiply uncontrollably. Under the microscope, however, there is no evidence of pooled trapped sebum.[original research?] Indeed the oil percolates through the plugged duct onto the surface. [citation needed] In response to the bacterial and yeast populations, the skin inflames, producing the visible lesion.
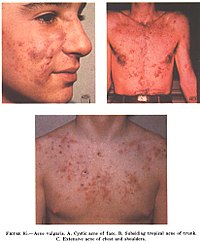
The face and upper neck are the most commonly affected, but the chest, back and shoulders may have acne as well. The upper arms can also have acne, but lesions found there are often keratosis pilaris, not acne. The typical acne lesions are: comedones, papules, pustules, nodules and inflammatory cysts known as cystic acne, one of the more severe forms. These are more inflamed and pus-filled or reddish bumps, that can easily lead to scarring or serious infections. Non-inflamed 'sebaceous cysts', more properly called epidermoid cysts, occur either in association with acne or alone but are not a constant feature. After resolution of acne lesions, prominent unsightly scars may remain.
Aside from scarring, its main effects are psychological, such as reduced self-esteem[3] and, according to at least one study, depression or suicide.[4] Acne usually appears during adolescence, when people already tend to be most socially insecure. Early and aggressive treatment is therefore advocated to lessen the overall impact to individuals.[3]
Causes of acne
There are many misconceptions and myths about acne. Exactly why some people get acne and some do not is not fully known. It is known to be partly hereditary. Several factors are known to be linked to acne:
- Family history
- Hormonal activity, such as menstrual cycles and puberty
- Stress, through increased output of hormones from the adrenal (stress) glands.
- Hyperactive sebaceous glands, secondary to the three hormone sources above.
- Accumulation of dead skin cells.
- Bacteria in the pores, to which the body becomes 'allergic'.
- Skin irritation or scratching of any sort will activate inflammation.
- Use of anabolic steroids.
- Any medication containing halogens (iodides, chlorides, bromides), lithium, barbiturates, or androgens.
- Exposure to high levels of chlorine compounds, particularly chlorinated dioxins, can cause severe, long-lasting acne, known as Chloracne.
Traditionally, attention has focused mostly on hormone-driven over-production of sebum as the main contributing factor of acne. More recently, more attention has been given to narrowing of the follicle channel as a second main contributing factor. Abnormal shedding of the cells lining the follicle, abnormal cell binding ("hyperkeratinization") within the follicle, and water retention in the skin (swelling the skin and so pressing the follicles shut) have all been put forward as important mechanisms. Several hormones have been linked to acne: the male hormones testosterone, dihydrotestosterone (DHT) and dehydroepiandrosterone sulfate (DHEAS), as well as insulin-like growth factor 1 (IGF-I). In addition, acne-prone skin has been shown to be insulin resistant [citation needed].
Development of acne vulgaris in later years is uncommon, although this is the age group for Rosacea which may have similar appearances. True acne vulgaris in adults may be a feature of an underlying condition such as pregnancy and disorders such as polycystic ovary syndrome or the rare Cushing's syndrome. Menopause-associated acne occurs as production of the natural anti-acne ovarian hormone estradiol fails at menopause. The lack of estradiol also causes thinning hair, hot flashes, thin skin, wrinkles, vaginal dryness, and predisposes to osteopenia and osteoporosis as well as triggering acne (known as acne climacterica in this situation).
Diet
There is no widely agreed-upon proof that diet has any effect on most people's acne. Eating greasy foods may get grease on a person's hands: subsequent contact of the hands to the face may exacerbate acne.
Milk
A recent study, based on a survey of 47,335 women, did find a positive epidemiological association between acne and consumption of partially skimmed milk, instant breakfast drink, sherbet, cottage cheese and cream cheese.[5] The researchers hypothesize that the association may be caused by hormones (such as several sex hormones and bovine IGF-I) present in cow milk. Although the association between milk and acne has been definitively shown, the ingredient in the milk responsible for the acne is still unclear. Most dermatologists are awaiting confirmatory research linking diet and acne but some support the idea that acne sufferers should experiment with their diets, and refrain from consuming such fare if they find such food affects the severity of their acne.[6]
Seafood
Seafood often contains relatively high levels of iodine. Iodine is known to make existing acne worse but there is probably not enough to cause an acne outbreak.[7] Still, people who are prone to acne may want to avoid excessive consumption of foods high in iodine.
High carbohydrates/High GI
It has also been suggested that there is a link between a diet high in refined sugars and other processed foods and acne. The theory is that rapidly digested carbohydrate food such as white bread and refined sugars produces an overload in metabolic glucose that is rapidly converted into the types of fat that can build up in sebaceous glands. According to this hypothesis, the startling absence of acne in non-westernized societies could be explained by the low glycemic index of these cultures' diets. Others have cited possible genetic reasons for there being no acne in these populations, but similar populations shifting to these diets do develop acne.[citation needed] Note also that the populations studied consumed no milk or other dairy products.[8] Further research is necessary to establish whether a reduced consumption of high-glycemic foods (such as soft drinks, sweets, white bread) can significantly alleviate acne, though consumption of high-glycemic foods should in any case be kept to a minimum, for general health reasons.[9] Avoidance of 'junk food' with its high fat and sugar content is also recommended.[10] On the other hand there is no evidence that fat alone makes skin oilier or acne worse.
One study [specify] suggested that chocolate, french fries, potato chips and sugar, among others, affect acne. A high GI (glycemic index) diet that causes sharp rises in blood sugar worsens acne. [11] If this study's conclusions are verified then a low GI diet may help acne also, but a 2005 review of somewhat dated scientific literature cannot affirm either way.[12] A study in November 2006 in Australia gave a 50% reduction in 12 weeks in mild-moderate facial acne by introducing its subjects to a high protein, low GI diet.[13]
Vitamins A and E
Studies have shown that newly diagnosed acne patients tend to have lower levels of vitamin A circulating in their bloodstream than those that are acne free.[14] In addition people with severe acne also tend to have lower blood levels of vitamin E.[15]
Hygiene
Acne is not caused by dirt. This misconception probably comes from the fact that blackheads look like dirt stuck in the openings of pores. The black color is simply not dirt but compact keratin[citation needed]. In fact, the blockages of keratin that cause acne occur deep within the narrow follicle channel, where it is impossible to wash them away. These plugs are formed by the failure of the cells lining the duct to separate and flow to the surface in the sebum created there by the body.
Sex
Common myths state that masturbation causes acne and, conversely, that celibacy or sexual intercourse can cure it.
Treatments
Overview of treatment
Acne can be divided into causes and symptoms.
The causes are mostly metabolic pressures from hormonal change and increased stress on the immune system due to lifestyle stress and artificial levels of toxins in the body. These can sometimes be improved through healthy lifestyle, low toxin low sugar natural diets, proper levels of exercise, situational organisation and improvements in stress levels, decent hygiene, gentle skincare, and in more serious cases there is a wide array of clinical methods such as drugs.
The symptoms results from an overactive or poorly drained stressed lymphatic system coping with toxins, sugars and bacteria, in the form of zits and pustules. To clinically treat acne if there is a buildup of pus that remains trapped with no way out after a week of the inflammation, it is far preferable to evacuate it with a sharp sterilised needle, penetrating into the skin and thus creating a channel, than by a sufferer bruising the area and damaging the tissues of the dermis. Also, antibacterial creams such as Savlon are able to lessen the state of an inflammation from the surface.
Timeline of acne treatment
The history of acne reaches back to the dawn of recorded history. In Ancient Egypt, it is recorded that several pharaohs were acne sufferers[citation needed]. From Ancient Greece comes the English word 'acne' (meaning 'point' or 'peak'). Acne treatments are also of considerable antiquity:
- Ancient Rome[citation needed]: bathing in hot, and often sulfurous, mineral water was one of the few available acne treatments. One of the earliest texts to mention skin problems is De Medicina by the Roman writer Celsus.
- 1800s: Nineteenth century dermatologists used sulphur in the treatment of acne. It was believed to dry the skin.
- 1920s: Benzoyl Peroxide is used
- 1930s: Laxatives were used as a cure for what were known as 'chastity pimples'. Radiation also was used.
- 1950s: When antibiotics became available, it was discovered that they had beneficial effects on acne. They were taken orally to begin with. Much of the benefit was not from killing bacteria but from the anti-inflammatory effects of tetracycline and its relatives. Topical antibiotics became available later.
- 1960s: Tretinoin (original Trade Name Retin A) was found effective for acne. This preceded the development of oral isotretinoin (sold as Accutane and Roaccutane) since the early 1980s.
- 1980s: Accutane is introduced in America
- 1990s: Laser treatment introduced
- 2000s: Blue/red light therapy
Some old treatments, like laxatives, have fallen into disuse but others, like spas, are recovering their popularity
Available treatments
There are many products sold for the treatment of acne, many of them without any scientifically-proven effects. Generally speaking successful treatments give little improvement within the first week or two; and then the acne decreases over approximately 3 months, after which the improvement starts to flatten out. Treatments that promise improvements within 2 weeks are likely to be largely disappointing. Short bursts of cortisone, quick bursts of antibiotics and many of the laser therapies offer a quick reduction in the redness, swelling and inflammation when used correctly, but none of these empty the pore of all the materials that trigger the inflammation. Emptying the pores takes months. [citation needed]
Modes of improvement are not necessarily fully understood but in general treatments are believed to work in at least 4 different ways (with many of the best treatments providing multiple simultaneous effects):
- normalising shedding into the pore to prevent blockage
- killing P. acnes
- antinflammatory effects
- hormonal manipulation
A combination of treatments can greatly reduce the amount and severity of acne in many cases. Those treatments that are most effective tend to have greater potential for side effects and need a greater degree of monitoring, so a step-wise approach is often taken. Many people consult with doctors when deciding which treatments to use, especially when considering using any treatments in combination. There are a number of treatments that have been proven effective:
Exfoliating the skin
This can be done either mechanically, using an abrasive cloth or a liquid scrub, or chemically. Common chemical exfoliating agents include salicylic acid and glycolic acid, which encourage the peeling of the top layer of skin to prevent a build-up of dead skin cells which combine with skin oil to block pores. It also helps to unblock already clogged pores.[citation needed] Note that the word "peeling" is not meant in the visible sense of shedding, but rather as the destruction of the top layer of skin cells at the microscopic level. Depending on the type of exfoliation used, some visible flaking is possible. Moisturizers and anti-acne topicals containing chemical exfoliating agents are commonly available over-the-counter. Mechanical exfoliation is less commonly used as many benefits derived from the exfoliation are negated by the act of mechanically rubbing and irritating the skin.

Topical bactericidals
Widely available OTC bactericidal products containing benzoyl peroxide may be used in mild to moderate acne. The gel or cream containing benzoyl peroxide is rubbed, twice daily, into the pores over the affected region. Bar soaps or washes may also be used and vary from 2 to 10% in strength. In addition to its therapeutic effect as a keratolytic (a chemical that dissolves the keratin plugging the pores) benzoyl peroxide also prevents new lesions by killing P.acnes. Unlike antibiotics, benzoyl peroxide has the advantage of being a strong oxidizer (essentially a mild bleach) and thus does not appear to generate bacterial resistance. However, it routinely causes dryness, local irritation and redness. A sensible regimen may include the daily use of low-concentration (2.5%) benzoyl peroxide preparations, combined with suitable non-comedogenic moisturisers to help avoid overdrying the skin.[16]
Care must be taken when using benzoyl peroxide, as it can very easily bleach any fabric or hair it comes in contact with.
Other antibacterials that have been used include triclosan, or chlorhexidine gluconate but these are often less effective.

topical antibiotics
Externally applied antibiotics such as erythromycin, clindamycin, Stiemycin or tetracycline aim to kill the bacteria that are harbored in the blocked follicles. Whilst topical use of antibiotics is equally as effective as oral, this method avoids possible side effects of stomach upset or drug interactions (e.g. it will not affect the oral contraceptive pill), but may prove awkward to apply over larger areas than just the face alone.
Oral antibiotics
Oral antibiotics used to treat acne include erythromycin or one of the tetracycline antibiotics (tetracycline, the better absorbed oxytetracycline, or one of the once daily doxycycline, minocycline or lymecycline). Trimethoprim is also sometimes used (off-label use in UK). However, reducing the P. acnes bacteria will not, in itself, do anything to reduce the oil secretion and abnormal cell behaviour that is the initial cause of the blocked follicles. Additionally the antibiotics are becoming less and less useful as resistant P. acnes are becoming more common. Acne will generally reappear quite soon after the end of treatment—days later in the case of topical applications, and weeks later in the case of oral antibiotics.
It has been found that sub-antimicrobial doses of antibiotics such as minocycline also improve acne. It is believed that minocycline's anti-inflammatory effect also prevents acne. These low doses do not kill bacteria and hence cannot induce resistance.
Hormonal treatments
In females, acne can be improved with hormonal treatments. The common combined oestrogen/progestogen methods of hormonal contraception have some effect, but the anti-testosterone, Cyproterone, in combination with an oestrogen (Diane 35) is particularly effective at reducing androgenic hormone levels. Diane-35 is not available in the USA, but a newer oral contraceptive containing the progestin drospirenone is now available with fewer side effects than Diane 35 / Dianette. Both can be used where blood tests show abnormally high levels of androgens, but are effective even when this is not the case. Along with this, treatment with low dose spironolactone can have anti-androgenetic properties, especially in patients with polycystic ovarian syndrome.
If a pimple is large and/or does not seem to be affected by other treatments, a dermatologist may administer an injection of cortisone directly into it, which will usually reduce redness and inflammation almost immediately. This has the effect of flattening the pimple, thereby making it easier to cover up with makeup, and can also aid in the healing process. Side effects are minimal, but may include a temporary whitening of the skin around the injection point. This method also carries a much smaller risk of scarring than surgical removal.
Topical retinoids
Normalizing the follicle cell lifecycle. A group of medications for this are topical retinoids such as tretinoin (brand name Retin-A), adapalene (brand name Differin) and tazarotene (brand name Tazorac). Like isotretinoin, they are related to vitamin A, but they are administered as topicals and generally have much milder side effects. They can, however, cause significant irritation of the skin. The retinoids appear to influence the cell creation and death lifecycle of cells in the follicle lining. This helps prevent the hyperkeratinization of these cells that can create a blockage. Retinol, a form of vitamin A, has similar but milder effects and is used in many over-the-counter moisturizers and other topical products. Effective topical retinoids have been in use over 30 years but are available only on prescription so are not as widely used as the other topical treatments. Topical retinoids often cause an initial flare up of acne and facial flushing (physiology).
Oral retinoids
Reducing the secretion of oils from the glands. This is done by a daily oral intake of vitamin A derivatives like isotretinoin (marketed as Accutane, Sotret, Claravis) over a period of 4-6 months. It is believed that isotretinoin works primarily by reducing the secretion of oils from the glands, however some studies suggest that it affects other acne-related factors as well. Isotretinoin has been shown to be very effective in treating severe acne and can either improve or clear well over 80% of patients. The drug has a much longer effect than anti-bacterial treatments and will often cure acne for good. The treatment requires close medical supervision by a dermatologist because the drug has many known side effects (many of which can be severe). About 25% of patients may relapse after one treatment. In those cases, a second treatment for another 4-6 months may be indicated to obtain desired results. It is often recommended that one lets a few months pass between the two treatments, because the condition can actually improve somewhat in the time after stopping the treatment and waiting a few months also gives the body a chance to recover. Occasionally a third or even a fourth course is used, but the benefits are often less substantial. The most common side effects are dry skin and occasional nosebleeds (secondary to dry nasal mucosa). Oral retinoids also often cause an initial flare up of acne within a month or so, which can be severe. There are reports that the drug has damaged the liver of patients. For this reason, it is recommended that patients have blood samples taken and examined before and during treatment. In some cases, treatment is terminated due to elevated liver enzymes in the blood, which might be related to liver damage. Others claim that the reports of permanent damage to the liver are unsubstantiated, and routine testing is considered unnecessary by some dermatologists. Blood triglycerides also need to be monitored. However, routine testing are part of the official guidelines for the use of the drug in many countries. Some press reports suggest that isotretinoin may cause depression but as of September 2005 there is no agreement in the medical literature as to the risk. The drug also causes birth defects if women become pregnant while taking it or take it while pregnant. For this reason, female patients are required to use two separate forms of birth control or vow abstinence while on the drug. Because of this, the drug is supposed to be given to females as a last resort after milder treatments have proven insufficient. Restrictive rules (see iPledge Program) for use were put into force in the USA beginning in March 2006 to prevent misuse.[17] This has occasioned widespread editorial comment.[18]
Phototherapy
'Blue' and red light
It has long been known that short term improvement can be achieved with sunlight. However, studies have shown that sunlight worsens acne long-term, as the skin's natural reaction is to produce more oils. [citation needed] More recently, visible light has been successfully employed to treat acne (Phototherapy) - in particular intense violet light (405-420nm) generated by purpose-built fluorescent lighting, dichroic bulbs, LEDs or lasers. Used twice weekly, this has been shown to reduce the number of acne lesions by about 64%;[19] and is even more effective when applied daily. The mechanism appears to be that a porphyrin (Coproporphyrin III) produced within P. acnes generates free radicals when irradiated by 420nm and shorter wavelengths of light.[20] Particularly when applied over several days, these free radicals ultimately kill the bacteria.[21] Since porphyrins are not otherwise present in skin, and no UV light is employed, it appears to be safe, and has been licensed by the U.S. FDA.[22] The treatment apparently works even better if used with red visible light (660 nanometer) resulting in a 76% reduction of lesions after 3 months of daily treatment for 80% of the patients;[23] and overall clearance was similar or better than benzoyl peroxide. Unlike most of the other treatments few if any negative side effects are typically experienced, and the development of bacterial resistance to the treatment seems very unlikely. After treatment, clearance can be longer lived than is typical with topical or oral antibiotic treatments; several months is not uncommon. The equipment or treatment, however, is relatively new and reasonably expensive. The equipment can be found in dermatologist offices but is moving towards personal portable devices. There are currently a number of brands coming out with hand held devices that are more affordable but not as powerful.
Photodynamic therapy
In addition, basic science and clinical work by dermatologists Yoram Harth and Alan Shalita and others has produced evidence that intense blue/violet light (405-425 nanometer) can decrease the number of inflammatory acne lesion by 60-70% in 4 weeks of therapy, particularly when the P.acnes is pretreated with delta-aminolevulinic acid (ALA), which increases the production of porphyrins. However this photodynamic therapy is controversial and apparently not published in a peer reviewed journal.
Less widely used treatments
- Azelaic acid (brand names Azelex, Finevin, Skinoren) is suitable for mild, comedonal acne.[24]
- Zinc: Orally administered zinc gluconate has been shown to be effective in the treatment of inflammatory acne, although less so than tetracyclines.[25][26]
- Tea Tree Oil (Melaleuca Oil) has been used with some success, and has been shown to be an effective anti-inflammatory in skin infections. [27][28][29]
- Nicotinamide, (Vitamin B3) used topically in the form of a gel, has been shown in a 1995 study to be more effective than a topical antibiotic used for comparison, as well as having fewer side effects.[30] Topical nicotinamide is available both on prescription and over-the-counter. The property of topical nicotinamide's benefit in treating acne seems to be its anti-inflammatory nature. It is also purported to result in increased synthesis of collagen, keratin, involucrin and flaggrin.[citation needed]
- There are also certain treatments for acne mentioned in Ayurveda using herbs such as Aloe vera,[31] Aruna, Haldi (Turmeric),and Papaya.[32] There is limited evidence from conventional medical studies on these products.[27] Products from Rubia cordifolia, Curcuma longa (commonly known as Turmeric), Hemidesmus indicus (known as ananthamoola or anantmula), and Azadirachta indica (Neem) have been shown to have anti-inflammatory effects, but not aloe vera.[33]
- Rofecoxib was shown to improve premenstrual acne vulgaris in a placebo controlled study.[34]
- Microdermabrasion uses crystals to exfoliate the top layer of the skin, allowing trapped bacteria to be purged. Probably the single biggest advantage that microdermabrasion has over alternative skin treatments is that a microdermabrasion patient can return to normal daily activities after receiving the treatment.[35]
Laser treatment
Laser surgery has been in use for some time to reduce the scars left behind by acne, but research has been done on lasers for prevention of acne formation itself. The laser is used to produce one of the following effects:
- to burn away the follicle sac from which the hair grows
- to burn away the sebaceous gland which produces the oil
- to induce formation of oxygen in the bacteria, killing them
Since lasers and intense pulsed light sources cause thermal damage to the skin there are concerns that laser or intense pulsed light treatments for acne will induce hyperpigmented macules (spots) or cause long term dryness of the skin.
The FDA has approved several companies, such as Candela Corp. to use a cosmetic laser for the treatment of acne.[36] However, efficacy studies have used very small sample sizes (fewer than 100 subjects) for periods of six months or less, and have shown contradictory results.[1],[2] Also, laser treatment being relatively new, protocols remain subject to experimentation and revision,[3], and treatment can be quite expensive. Also, some Smoothbeam laser devices had to be recalled due to coolant failure, which resulted in painful burn injuries to patients.[4]
Future treatments
Because acne appears to have a significant hereditary link, there is some expectation that cheap whole-genome DNA sequencing may help isolate the body mechanisms involved in acne more precisely, possibly leading to a more satisfactory treatment. (Crudely put, take the DNA of large samples of people with significant acne and of people without, and let a computer search for statistically strong differences in genes between the two groups). However, as of 2007, DNA sequencing is not yet affordable for most, and all this may still be decades off. It is also possible that gene therapy could be used to alter the skin's DNA.
Phage therapy has been proposed to kill P. acnes, and has seen some use, particularly in Georgia.[37]
Preferred treatments by types of acne vulgaris
- Comedonal (non-inflammatory) acne: local treatment with azelaic acid, salicylic acid, topical retinoids, benzoyl peroxide.
- Mild papulo-pustular (inflammatory) acne: benzoyl peroxide or topical retinoids, topical antibiotics (such as erythromycin).
- Moderate inflammatory acne: benzoyl peroxide or topical retinoids combined with oral antibiotics (tetracyclines). Isotretinoin is an option.
- Severe inflammatory acne, nodular acne, acne resistant to the above treatments: isotretinoin, or contraceptive pills with cyproterone for females with virilization or drospirenone.
Acne scars
Severe acne often leaves small scars where the skin gets a "volcanic" shape. Acne scars are difficult and expensive to treat, and it is unusual for the scars to be successfully removed completely.[citation needed]
Physical acne scars are often referred to as "Icepick" scars. This is because the scars tend to cause an indentation in the skin's surface. There are a range of treatments available.
Although quite rare, the medical condition Atrophia Maculosa Varioliformis Cutis results in "acne like" depressed scars on the face.

Ice pick scars - Deep pits, that are the most common and a classic sign of acne scarring.
Box car scars - Angular scars that usually occur on the temple and cheeks, and can be either superficial or deep, these are similar to chickenpox scars.
Rolling scars - Scars that give the skin a wave-like appearance.
Hypertrophic scars - Thickened, or keloid scars. [38]
Pigmentation
Pigmented scars is a slightly misleading term, suggesting a change in the skin's pigmentation, and that they are true scars. Neither is true. Pigmented scars are usually the result of nodular or cystic acne (the painful 'bumps' lying under the skin). They often leave behind an inflamed red mark. Often, the pigmentation scars can be avoided simply by avoiding aggravation of the nodule or cyst. When sufferers try to 'pop' cysts or nodules, pigmentation scarring becomes significantly worse, and may even bruise the affected area. Pigmentation scars nearly always fade with time taking between 3 months to two years to do so, although rarely can persist.
On the other hand, some people, particularly people with naturally tanned skin do develop brown hyperpigmentation scars which is caused by a local increased production of the pigment melanin. These too typically fade over time.
Grading scale
There are multiple grading scales for grading the severity of acne vulgaris,[39] three of these being: Leeds acne grading technique: Counts and categorises lesions into inflammatory and non-inflammatory (ranges from 0-10.0). 'Cook's acne grading scale: Uses photographs to grade severity from 0 to 8 (0 being the least severe and 8 being the most severe). Pillsbury scale: Simply classifies the severity of the acne from 1 (least severe) to 4 (most severe).
Pimple
A pimple is a result of a blockage of the skin's pore. See Acne vulgaris.
Inside the pore are sebaceous glands which produce sticky sebum. When the outer layers of skin shed (as it does continuously), the dead skin cells left behind may become 'glued' together by the sticky sebum. This causes a blockage in the pore, especially when the skin becomes thicker at puberty[1]. The sebaceous glands produce more sebum which builds up behind the blockage, and this sebum harbours various bacteria including the species Propionibacterium acnes. Since the body's natural defence against bacteria is primarily phagocytes (white blood cells), these rush to the site behind the blockage (where the bacteria are). This is what gives some pimples the 'whiteheads' (unless the Phagocytes are deeper in the skin, which means you can't see the 'white' caused by them). The white blood cells then destroy (by phagocytosis) the bacteria to prevent infection. The pain one may feel when a pimple is present is caused by the widening of skin around the white blood cells.
Common over-the-counter medications for pimples are Benzoyl peroxide and/or salicylic acid. Both medications can be found in many creams and gels used to treat acne through topical application. Both medications help skin slough off easier, which helps to remove bacteria faster. A regimen of keeping the affected skin area clean plus the regular application of these topical medications is usually enough to keep acne under control, if not at bay altogether. 1-2% of the population is allergic to Benzoyl peroxide treatments. Severe acne usually indicates the necessity of prescription medication to treat pimples. Prescription medications used to treat acne include isotretinoin, which is a retinoid. Historically, antibiotics such as tetracyclines and erythromycin were prescribed. While they were more effective than topical applications of benzoyl peroxide, the bacteria eventually grew resistant to the antibiotics and the treatments became less and less effective. Also, antibiotics had more side effects than topical applications (erythromycin can cause stomach cramps)Stop Squeezing Your Pimples - 7 Safe Ways to Get Rid of Pimples
It’s everyone’s worst nightmare. Waking up the day before a special event to discover a big, red pimple baring itself for all to see right on your face!
Here’s how to get rid of it quickly and safely:
1. Don’t ever pinch, squeeze or pick at a pimple. This only causes it to become more red and inflamed, and will spread the bacteria and oils that caused it in the first place, to other parts of your face! It can also lead to scars.
2. Every 30 minutes, apply an ice pack to the pimple and hold it there for about 2 minutes. This will decrease the swelling and redness and help shrink the inflammation and pain that sometimes comes along with it.
3. They don’t call it concealer for nothing! Covering the pimple with a light dose of flesh-tinted concealer can help mask it when you’re in a hurry. It also helps cover up that oily shine.
4. Cleanse your skin 2-3 times a day with mild, unscented soap or a specialized acne cleanser that has no harsh chemicals (such as lye). Scrub skin gently with an exfoliating pad or washcloth, but don’t rub too hard, otherwise you’ll sap your skin of its own natural oils, which help to repel buildup naturally.
5. Apply a cream or ointment containing benzyl peroxide or salicylic acid (many over-the-counter acne medicines contain these ingredients) to the blemish or around the entire facial area. Note that these ingredients both have a tendency to dry out skin if used too much and are not recommended if you have sensitive skin.
6. Wear oil-free makeup whenever possible. These types have less of a tendency to cause the pore buildup that results in blemishes. Remove your makeup nightly and cleanse with an acne-fighting medicine to remove dirt, oil and makeup from deep within the skin.
7. If you’re in need of a quick fix, a dab of toothpaste on the affected area right before bed can help soothe irritation and reduce redness. Pressing and holding a wet tea bag or a cotton ball with a dab of lemon juice against the blemish for five minutes can also reduce swelling and redness.
If you follow these tips, chances are you’ll notice a significant difference rather quickly – often within a day or two. If pimples become a recurring problem or worsen, your doctor or dermatologist can suggest a daily skin cleansing routine that will suit your skin type. Other long-term remedies, such as facial masks, diet adjustments and increasing the amount of water you drink can also help combat outbreaks.
The information contained in this article is for educational purposes only and is not intended to medically diagnose, treat or cure any disease. Consult a health care practitioner before beginning any health care program.
How To Cure Sensitive Teeth
I figured out what it was when I went on a journey and left my electric toothbrush at home. After a couple of days the headache was gone, but when I got home and started to use the electric toothbrush again it soon reappeared.
Now I only use the (in regards to dental hygiene, superior) electric toothbrush a few times each week and the headache stays away.
It's no funny thought, but I wonder if one could sustain brain damage if exposed to the vibrations of electric toothbrushes too often.
The reason why I started to use an electric toothbrush was that hard toothbrushes disappeared from the market a few years ago, and hard toothbrushes were the only means I knew of which effectively kept tartar off my teeth. For a while I even used a kind of toothbrushes meant to clean prosthetics (brushes which were hard enough to clean the ownen with) before I discovered that electric toothbrushes were just as good, or even better, at cleaning the teeth.
The reason that hard toothbrushes are removed from most markets was that some people damaged their gum with them, causing gingival recession, which in turn caused hypersensitivity and in worst cases loss of teeth. That brushing alone should count for loss of enamel or cementum though, is a myth.
I've never experienced such problems, nor cavities and similar either, despite that I used hard toothbrushes for more than 15 years, and the reason for that is how I brush my teeth.
If you wish to be spared from hypersensitivity in your teeth then the angle you hold your toothbrush is the most important thing to keep in mind; you should brush your teeth "with the fur" and never hold the brush so that the bristles can tear into the gum. You shouldn't either brush your teeth more than twice a day, do instead complement with fluoride rinse and xylitol chewing gum.
That's it, no cavities and no more hypersensitivity - it's (usually) as easy as that.

Brush in this manner and sensitive teeth comes with a guarantee.
The gum gets weared and the dentin (dentin is a mineralized connective tissue which makes up most of the tooth's root) becomes exposed, and the nerves within reacts so that you feel a shooting pain, especially when you consume cold and acidic stuff.

If you brush this way you will probably not experience sensitive teeth.
After a while you can chew popsicles just as when you were a kid (and all the grown-ups got the shivers when seeing you doing it).
Sensitive teeth gel or sensitivity protection toothpaste is as you can see no cure, but can help during the time the gum is healing. Pain-relieving toothpaste could actually worsen the situation if you continue to brush your teeth in a wrongful manner, since you won't notice the damage done as much as you should have done without the pain-killer.
Cure acne - get rid of pimples
You do not get acne from chocolate or strong spices. Or, yes, you will get acne from chocolate, but not because you eat it. You get pimples because you touch yourself in the face when you eat chocolate. When you poke around in your face with dirty fingers - you might have a habit of leaning your head against your hand or stroke your chin when you think - you are massaging bacteria and dirt into sensitive pores which will then turn into pimples.
You could also suffer from acne as a symptom of (usually) intestinal problems. If you get pimples in symmetrical patterns in your face, especially along the jawlines, it can be either a symptom of IBS - Irritated Bowel Syndrome - colon irritabile, that you stress to much and thus upset your stomach, or that you eat things that aren't good for you - or all of those alternatives. The article on heartburn might help you put a stop to such acne.
Follow these advises in order to get rid of pimples:
- Stop touching your face. See to that areas where you have acne aren't covered or irritated by shirt-collars or caps - especially not dirty such.
- Do not dry out the skin. Do not wash your skin with dehydrating anti-acne solutions. Such solutions cause the skin to produce more fat which in turns increases the risk of blocking the skin's pores.
- Wash your face with pure water only - do not use soap or alcohol based solutions. Do not rinse your face with cold water after shaving in order to "close the pores" - let them breathe instead.
- Do not shave yourself the wrong way. Shave in the same direction as the hairs grow. If you shave in the opposite direction you will cut off small pieces of the skin which is lifted up with the hairs. The sore skin will then probably get infected - it's far better with bristles than red pus-filled spots.
- Carefully squeeze pus-filled pimples. It's more likely that you will get worse scars from suppurations that are left to heal for themselves than from cleaned out "craters". Do use lots of disinfectants though and powder the wound with non-scented baby powder or similar in order to keep it dry and clean.
- Use a skin lotion which contains carbamide in order to keep your skin moisturized after you washed yourself. Carbamide tunes your skin's moisture balance in a natural way. Eventually you could mix in some weak cortisone-gel if your skin is irritated.
- Sunbathe. Adequate exposure to the sun helps the body to create vitamin D which is good for the immune system.
- Exercise and take a sauna. The skin needs to sweat - don't be afraid of that - in order to get clean in depth.
And remember - the pimple is always worst in the mirror you are looking in.